Early on in 2020, I had a breakdown, which is exactly how I’d expect myself to prelude a pandemic.
I’ve always been a bit of an extremist. Until recently, I left little space for gray areas. I suppose those closest to me would say that I don’t half-ass anything, which has afforded me many opportunities while also laying the foundation for what folks now call “burnout.” My loved ones would also probably acknowledge that, though the last few years have brought life lessons to show me the gradient, I’m not completely over the hump of the all-or-nothing mindset.
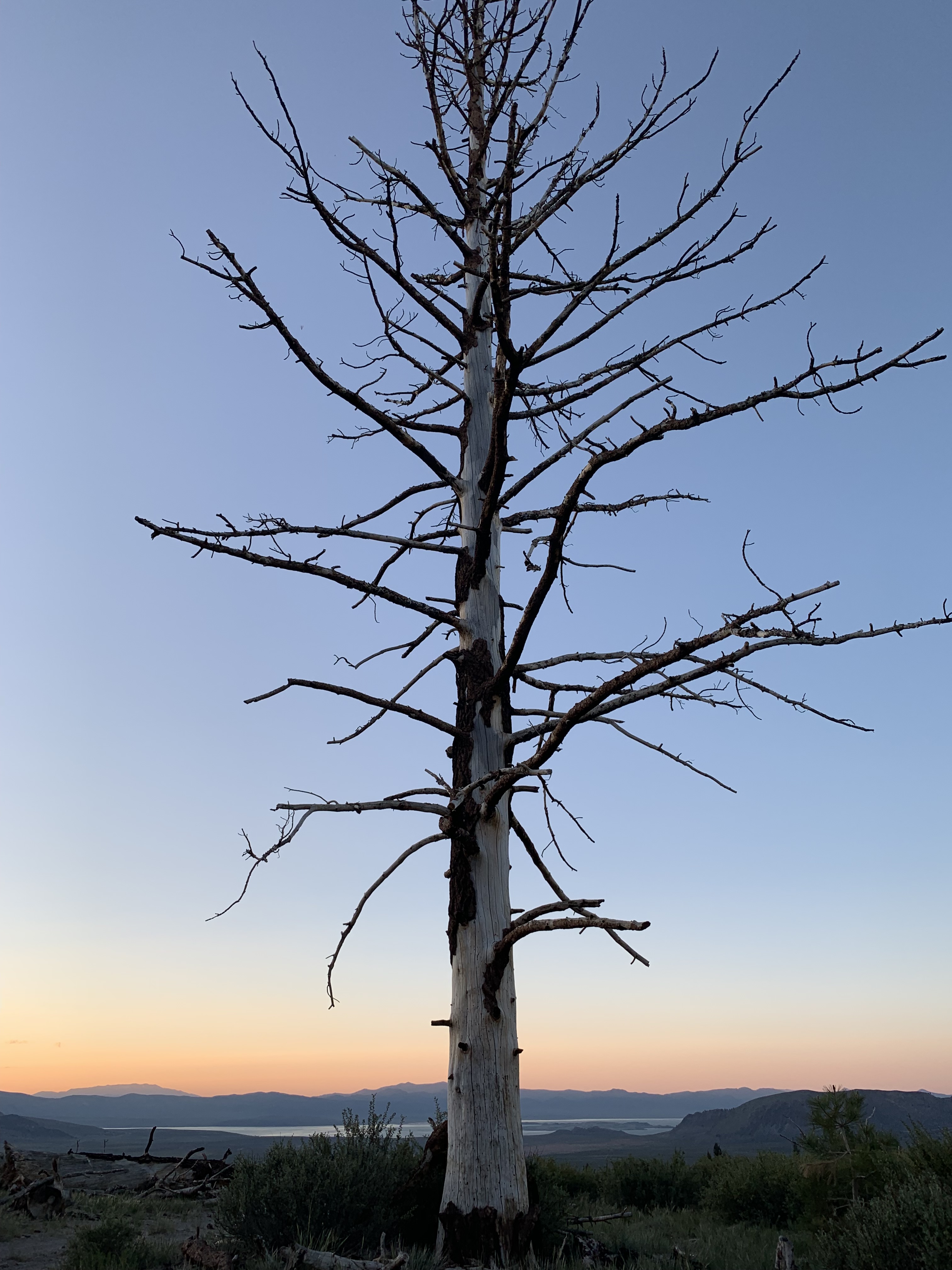
For example, late in 2014 I started feeling like I needed a change. So, I began silently scheming. Come June of 2015, I rid myself of most of my belongings. I left my familiar life close to my roots to embark on a solo journey around the western states, living in a tent. If you know me, you likely know this story. Unbeknownst to me, three and a half years of continuous travel would follow this departure. Whatever prompted this ambition and gumption to initiate and sustain a lifestyle change like this is a mystery to me. However, I suspect this mystery may also be the birthplace of my emotional distress. But let’s back up a bit to my earlier years.
As a teenager, I trialed medications for my mental health. There was never a consistent diagnosis. There had been suspicion of a mood disorder but the only certainty was in my struggle with anxiety and depression. At a later point, there was an OCD diagnosis that also didn’t seem to stick. Seeing psychiatrists can be like Forrest Gump’s box of chocolates.
Somewhere around the start of college, I landed on Lexapro, an antidepressant. My current doctor has disclosed that Lexapro is considered a relatively mild SSRI, but I learned in recent years that it was the culprit of the relentless night sweats I (and my partners over the years) mysteriously endured for over ten years. It wasn’t just during slumber, either. It was typical for me to have beads of sweat trickling down the insides of my arms consistently throughout the day. I could be indoors, underdressed and sedentary and it still happened. My doctors either came up empty handed or hypothesized birth control as the culprit.
I started accepting this as part of my chemical makeup, especially after relinquishing birth control to no avail. I then visited my parents’ doctor, having just arrived back in the U.S. from living abroad. When I told him about the years of night sweats and relentless perspiration in general, he nodded and nonchalantly replied with:
“Oh, yes, Lexapro will do that.”
He continued on in conversation as if this was common knowledge. Turns out, this is a common side effect of SSRIs, which was just somehow overlooked in my case. For over a decade.
Even while on Lexapro I experienced crippling episodes of anxiety along with bouts of depression. To make matters worse, I experienced a slew of unfortunate events that stretched from 2018 to 2019, which happened to be a time I was trying to work myself off of Lexapro. I had come back to the U.S. earlier than planned from my travels in 2018 as I had been chronically ill with what we soon discovered was Lyme Disease; that diagnosis came Fall of 2018.
It’s worth noting my stubbornness in still wanting to relieve myself of Lexapro while my health was unstable. In addition to the Lyme diagnosis, there was also a devastating breakup after an infidelity, the adjustment back to “normal” life with the international relocation, and within it all, a whole lot of therapy.
This was tragically followed by the suicide of a loved one a few months later, which resulted in what my therapist calls “complicated grief.” Clearly, not an ideal time to be working myself off medication that was assisting with my emotional stability. Nonetheless, I continued onward as I didn’t see at the time that maybe I shouldn’t have been adding another element to what was happening in my life. Or rather, taking one away…one that could have been keeping the camel’s back in place. Plus, there was that whole I-don’t-half-ass-anything piece to the puzzle, along with the stigma attached to antidepressants which I took issue with.
My track record with side effects certainly played a role as well. I wanted to do things the natural way by taking ashwagandha and magnesium, by meditating, utilizing movement therapies and other therapies of varying kinds. I had been working on this since 2016, when I decided to go the Naturopathic and Integrative Medicine route.
To add yet another component, I was also in an escalating existential crisis (I know, I know, there’s a lot here, but we’ll get there, I promise; and it’s not all bad!). I realized that the work I had been doing for over a decade wasn’t fulfilling. This became apparent to me after coming back to the states where I readjusted to living in one place, with four walls, and was no longer transient. I had essentially only been doing the work because it allowed me to travel and work remotely. It was available to me and I was good at it. I was very grateful for this, but gratitude couldn’t make it align with my core values.
I suppose a breakdown was the appropriate step to follow all of this, and in March of 2020, it was just in time for COVID-19 to commence. As the psychiatrist I was about to seek out (Dr. P) phrased it, I had been “crashing and burning” for some time. He made this statement based on the history I gave…I’m so glad I could provide all that useful information. I found his statement ironic given that I had a psychiatrist in college that used a house burning to the ground as an analogy for the necessity of being proactive:
“You don’t wait until the house is burnt down to call the fire department, Molly.”
No shit.
She had been referring to my deteriorating emotional well-being. My Mom would revisit this quote in June of 2020, a few months after my breakdown, but we’ll get to that later.
Back to Spring of 2020…
Post-breakdown it was time to find a psychiatrist. A new one that is, as the last one I had seen didn’t quite work out. I knew her for maybe four months, and she was the first psychiatrist I had seen in over a decade. Having been on Lexapro for so long, I was told that medication upkeep was left to a primary care physician. These were annual visits where the general practitioner would ask if the medication was “working for me” to which I’d respond, “I think so?” Then I’d get blood drawn for a basic metabolic panel, they’d have a quick glimpse at my vagina, then check my breasts for lumps, and sianara.
I remember when I lived in Australia I went to see a gynecologist for what I correctly suspected to be a yeast infection (if that sentence made you cringe, my essays are probably not for you). The first thing she asked was about my diet. This was the first time I ever had a gynecologist ask me about my diet, and I was thirty. I had been drinking more wine than I ever had in my life and eating cheese regularly for the first time in years. Turns out, she suspected these factors to be the culprit. I digress.
The mentioned psychiatrist I saw for a few months had prescribed me an anti-anxiety medication, Buspirone, and an SSRI, Wellbutrin. I had been on Wellbutrin years before for smoking cessation. She gave me these because I had been experiencing panic attacks, which was new for me and an awful experience. Both she and my therapist believed this onset was due to Andy’s recent suicide. When these medications didn’t seem to help and I was concerned about their escalating side effects (especially when she threw Lorazepam into the mix), I scheduled an appointment to see her.
She was surprised to see me as it wasn’t yet time for us to follow up. When I voiced my concerns, she sure made me feel small. She told me that I was just a worrier and needed to worry less; that I was just weary of medication. She instructed that I get off the medication to see what “ground zero” looked like.
Well, I hit ground zero, lady.
I had half a mind to give her a ring after I found the new psychiatrist, Dr. P, and within his realm of possible diagnoses was Bipolar type 2 or mixed manic depression. Maybe I’d just inform her that she may have instructed someone with a serious mood disorder to cease medications without further follow up while oversimplifying and minimizing their pain to just worrying too much. Of course, I did not do this, but I found great satisfaction in the condescending thought. She was a monotone, patronizing woman…it could have in fact been her dullness that caused the whole damn thing!
She wasn’t the only doctor in my life with an opinion that Summer. My Naturopathic doctor had just apologetically taken me off two medications, treating an underactive thyroid and overactive adrenal glands, whose side effects didn’t bode well for me, either. She was more compassionate:
“You’re having an existential crisis, the life you have isn’t working for you, we need to get you a new one.”
No pressure.
All humor aside, the new psychiatrist suspected bipolar type two, mixed manic depression or cyclothymia as possible diagnoses. He also noted that it was obvious Doctors had been “putting me through the ringer” for years. Given his diagnostic suspicion, it was time to test his theory, which meant medication trial and error. I would say this is my least favorite part of having a mental health condition. Psychiatry is apparently just as much an art as it is a science. There was also a smidge of irony in medication trial and error following his statement about having been put through the ringer…
Rather than say “bipolar type 2, mixed manic depression or cyclothymia” moving forward, I’m just going to say the bipolar spectrum or a bipolar disorder. I understand that bipolar isn’t seen as having a spectrum in the traditional sense by professionals and that it’s instead viewed as very black and white–but I tend to believe (now) that life is composed of a hell of a lot of gray areas. Plus, this is a personal essay, not a scientific journal, so I’m taking these liberties.
Latuda was the medication at the forefront of Dr. P’s mind and soon, the forefront of my bedtime routine, as was the required minimum intake of 350 calories (unfortunately beer didn’t count and was strongly discouraged). Getting to this point looked like several weekly or twice weekly conversations with the doc, at which point he explained his theory. He said that some people can have the chemical makeup for a bipolar disorder and:
“…go years highly functioning, even thriving, but then something happens; grief, an illness, a trauma, and it triggers.”
At this point he was talking slowly and with intent, looking at me as if he was talking about me personally. Then he actually said:
“I believe this is you.”
My mind was immediately flooded with thoughts of how I could have supposedly gone the rest of my life as a fly-under-the-radar bipolar type, but no! Life had to throw me every triggering example he provided! Once my pathetic “woe is me” moment was over, I refocused my attention. As the saying goes,
Gautama Buddha
He said that antidepressants alone can make people diagnosed as bipolar worse; the medication can make them hypomanic or manic (depending on Bipolar 1 or Bipolar 2) and that he has been doing this long enough to have learned this lesson. Knowing I had been on Lexapro for well over a decade, he suspected that I had something on the bipolar spectrum and that Lexapro had been making me worse over time.
Well, isn’t that just frickin’ lovely, I thought, almost letting out a frustrating chuckle at the irony of it all.
I beat myself up a bit about the whole “Lexapro could have been making me worse” theory. However, being on that medication seemed right at that time given the information at hand and the instruction I was provided by my doctors. So…we won’t spend any more time on that.
Dr. P continued to say that he once had a patient that was like me; an extrovert (I’m convinced I’m an introvert, but we will let this go for now), who was very social and outgoing and people loved him.
Well, this is a nice change of pace, I thought.
He even went so far as to say that he was sure he would find me very charming if he met me at a party.
Now he’s talkin’ my language!
My balloon was soon deflated, and quickly, when he continued to say that his former patient was thriving on an antidepressant for bipolar 2 until Dr. P got a call that the patient was on an airplane, heading to “The MotherLand to save the world.”
Oh, for fucks’s sake.
I don’t believe in God, so who knows what my “Save The MotherLand” moment would look like; I did think a Patagonia trip would be more my style. I would hope that in my hypomanic moment, I would have the wherewithal not to call a psychiatrist to come rain on my parade, isn’t that sort of the point?
I do understand hypomania and mania to be very real and serious and not something to be taken lightly. But if I wasn’t able to find humor or lightheartedness in these moments, it wouldn’t be very authentic of me. It’s who I am.
“And if I laugh at any mortal thing, ‘Tis that I may not weep”
Lord Byron (aka some dude my Mom told me about)
Once my balloon was fully deflated, we had a discussion about mood stabilizers and antipsychotics, at which point that withered balloon wisped far, far away. My fret surrounding a medication classified as an “antipsychotic” felt very real to me at that moment.
Am I psychotic? I certainly don’t feel that way. Sure, maybe neurotic at times, but you know….a normal dose of crazy, right?
He explained that these medications alter how dopamine is released in the body, among other things, and that he’d like to test his theory by putting me on Latuda, a brand new (and expensive) antipsychotic. It was all very overwhelming and felt a bit test-rat-esque.
I wish we could get back to the whole “people love me at parties” conversation.
I agreed to Latuda and it wasn’t thirty minutes later that I had myself scared shitless on the medication’s website. It wasn’t just the side effect list; it was also the clearly stated warnings. Fortunately, I could check one warning off my immediate worry list: the increased death rate in dementia patients. Yikes.
I’m no rookie when it comes to research; I go straight to the source, then Mayo Clinic and then scholarly medical articles and case studies, if necessary. This time, I had only gotten to the medication’s website and it was nerve-wracking. My gut told me not to do it. My instincts felt strongly that this was a bad idea. Then, my rational mind spoke up:
“This is what you need to do, Molly. You at least need to try, keep an open mind.”
My family agreed. That’s when my real nightmare commenced.
After prescribing Latuda, Dr. P rapidly increased the dosage. In all fairness, he was trying to work against my crisis, but my body quickly disagreed, and let it be known. My depression and anxiety had been crippling, but so were the pharmaceuticals (along with the stress from working through the near constant “symptom or side effect” question). Considering that I was also living alone, the pandemic had quickly picked up speed, plus I was out of work and out of money…I was a mess. I was fortunate enough to have a strong support system made up of loved ones near and far; my family, my partner, dear friends. It was challenging for them too, and I often found myself turning inward. Everyone had their own struggles during that time, and I have always had a fear of being a burden.
My ruminations festered. The permanence of bipolar was looming over me; a lifetime of invasive medication and side-effect management. I was aware that when all was said and done, it would be manageable– that I would adapt and be more than fine. But the road ahead felt like a long, desolate one. I was overwhelmed and also fearful that I wouldn’t be able to get my employment and financial matters in order while on that road. Especially during the pandemic.
My first night on the medication, I woke up in the middle of the night from a muscle spasm in my left frontal shoulder. I barely blinked an eye at this.
Meh, what’s one muscle spasm?
Then, in the middle of the day, all of a sudden, I felt like I was going to pass out. There were strange sensations in my arms and legs and I saw my veins visibly spasming in my thigh and forearm.
I’m dehydrated, I just need water.
Gulp after gulp, nothing changed until my hands and fingers started trembling uncontrollably.
Is this low blood sugar? I used to throw up when I was hungry and I’d start shaking. Maybe that’s it.
I recalled having an electrolyte drink for the flu I had purchased on a CVS run when the pandemic first commenced, thinking it could come in handy (having no real idea what the fuck we were going to be dealing with). I drank the instructed serving. The shaking continued, and the sensation that I was going to pass out was suddenly overwhelming. My heart felt like it was pumping very slowly to a complete halt. My head was light and disoriented, dizzy, confused. In my delirium and self-doubt, my mind scrambled:
Get to your bed.
Is this a manifestation of anxiety?
Do I call 911? We’re in a pandemic. Is that a waste of resources? Am I overreacting?
What is safe and wise right now?
I don’t want to be a bother to medical staff.
Am I being dramatic?
Will they take me seriously given the medication I’m on?
Don’t let your personal insecurities about being on an antipsychotic cloud your judgement!
Is the antibiotic I’m on interacting with Latuda? The pharmacist said I could take them together.
Remember that neurosis I spoke of? Well, she was clearly showing her ugly mug. Remember those instincts I didn’t trust in taking the medication in the first place? I couldn’t get myself to trust them this time, either. In all fairness, it was an uncertain time for all–not a time I wanted to be having bizarre, unfamiliar symptoms. I was also alone in my apartment, without anyone to consult, feeling anxious and unwell. I knew that my partner was a little less than a thirty-minute drive away, when he would normally be two blocks down (he’s still pissed I didn’t call him).
I called my friend Lindsay who lived a few blocks down. While she was on her way over, I called urgent care and, as I should have known, they were unable to give medical advice. I was also sure to leave a message with my psychiatrists’ office to have my Doctor, or the doctor on call, or frankly anyone, get back to me. I received a callback five hours later.
Lindsay showed up with a blood pressure monitor and sodium pills. I was grateful that she was close by and knowledgeable in these matters, especially since I had no idea what was happening to me. She knew right away that it was my blood pressure not blood sugar. She has POTS.
Vasovagal syncope. Yes, I said vasovagal; something I had never heard of but made me think of Vaseline and vaginas, sounding a bit like a personal lubrication brand. Not quite. It’s a sudden drop in blood pressure.
I stumbled on another side effect after my sibling Mackenzie and I had been joking about mattresses. I had told Mackenzie that I vacuum my mattress from time to time to get the dog hair off. Kenz found this hysterical. One day, I decided to take a video of myself doing this, to send as a joke —sibling humor. To my surprise and disappointment, I was very obviously and bizarrely clenching my mouth and lips. Constantly! It looked very “meddy.” This made me incredibly insecure, even more so when it was captured yet again on another video. The doc categorized this second side effect as “Akathisia.”
After all of those instances, the doctor assured me that Latuda could help me if I gave my body time to adjust to it. So, I continued on Latuda. After I complied, the medication sent me sky high in the worst way. I have not, to my knowledge or my psychiatrist’s knowledge, ever experienced mania (or hypomania for that matter, now that I’m not believed to be Bipolar). Although, in my unprofessional opinion, the closest I’ve come was while on Latuda—and I’m not talking about those “can’t sleep cocaine nights” in my twenties either—this was unique.
I do get some credit for it being my body, right?
I would call my Mom and the next thing I knew, three hours would have passed by and she wouldn’t have gotten so much as three words in. My Mom finally forcefully interrupted me to make me listen to a question she had, hoping it would stop me from spiraling out of control.
I remember finding myself sitting on my living room floor with papers and crafts and just clutter all around, wondering how I got myself into so many partially completed projects. Normally, I’m absolutely terrible at starting a new task before completing the one before. It’s actually a problem at times because I struggle to compartmentalize tasks and have to finish what’s at hand to feel at ease enough to let it go and move onto the next. However, on this particular afternoon, I recognized that if I had been watching myself as a fly on the wall, I would have been horrified at the scrambling and inefficiency.
I was frazzled and impatient. The meds that were supposed to be fixing me were creating problems where there weren’t any. It honestly felt and appeared as though the medication was causing Bipolar traits. Sounds crazy, I know, but in any case, it wasn’t looking good for Dr. P’s bipolar theory.
On another afternoon not long after, I was walking the dog not even a block from the apartment when all of a sudden, I started feeling those familiar sensations like I was going to pass out. I feared I would faint right there on the sidewalk. It was that moment I decided I was done.
I walked back and once I got in the door I looked at my partner and said:
“I’m done with this medication.”
He replied immediately: :
“I think that’s a great idea.”
The only benefit I got out of Latuda was that it brought me out of my depression and sent me flying into getting a whole lot of shit partially done, with one or two things completely finished. So, thanks to Latuda, I put together a Tribute video for my Mom’s birthday with 40 participants. She said it was the most thoughtful gift she’s ever received. Silver lining, I suppose.
The month of June was approaching and Latuda was working its way out of my system. Though I wanted to be hopeful, that desolate road to bettering my mental health was only feeling longer and longer. I sought out a second psychiatric opinion as advised by my primary care doctor and recommended by my loved ones. I then found Dr. B, who you’ll hear about soon enough.
I was back to square one, and that analogy about the burning house resurfaced while on the phone with my Mom from over 2,000 miles away, amidst the pandemic:
“The house is burning, Molly. You need to tell Dr. B that you’re in a crisis. It’s time to come home, honey.”



Thank you for sharing this, i wish you all the best 🙂
Molly you are an amazing writer! Looking forward to reading more of your work! Thanks for being so raw. 😉
I’m so impressed with your candor. Makes the rest of us feel like it’s ok to not know how to feel at times.